In the mammary glands during pregnancy, changes occur that prepare them for the secretion of milk. Already during pregnancy, a drop of secretion - colostrum - can be squeezed out of the nipple. In the postpartum period, the main function of the mammary glands begins and reaches full bloom, but in the first days after childbirth, only colostrum is squeezed out of the nipples. Colostrum is a thick yellowish alkaline liquid containing protein, fat droplets, epithelial cells from glandular vesicles and milk ducts, and "colostrum bodies" - large rounded cells with fatty inclusions (Fig. 120, a). 120. Microscopic picture of milk and colostrum. a - colostrum, fat droplets and colostrum bodies are visible; 6 - milk, only fat bodies are visible. The question of the origin of these cells has not been finally resolved. Apparently, these are leukocytes containing phagocytosed droplets of emulsified fat; perhaps some of them are epithelial cells in a state of fatty degeneration. Colostrum is rich in proteins and salts; it has fewer carbohydrates than milk. In colostrum there are vitamins, enzymes, antibodies. Milk separation begins on the 2nd-3rd day after birth. Usually at this time, the mammary glands become rough and sensitive. With severe engorgement, there are bursting pains in the mammary glands, radiating to the axillary region, where sensitive nodules are sometimes felt - swollen rudimentary lobules of the mammary glands. The secretion of milk occurs as a result of complex reflex and hormonal influences. The process of milk formation is regulated by the nervous system and lactogenic (prolactin, luteotropic hormone) pituitary hormone. This hormone induces milk secretion after preparation of the breast parenchyma during pregnancy by estrogen hormone (development of the excretory ducts) and progesterone (proliferation in the alveoli). A well-known stimulating effect is exerted by thyroid and adrenal hormones, which act through the pituitary gland. The function of the mammary glands largely depends on the reflex effects associated with the act of sucking. Perhaps, in the mammary glands, in addition to milk, a substance is formed that enhances the contractility of the uterus and contributes to its involution in the postpartum period. Uterine contractions also occur reflexively due to irritation of the nerve elements of the nipples when the baby suckles the breast. Reflex contraction of the uterus during feeding is often felt by the puerperal in the form of contractions. Milk is a white liquid, which is a suspension (emulsion) of tiny droplets of fat found in the whey (Fig. 120b). Milk is alkaline and does not coagulate when boiled. Its composition: water 87-88%, protein 1.5% (albumin, globulins, casein), fat 3.5-4.5%, carbohydrates (lactase) about 6.5-7%. salts 0.18-0.2%. Milk, like colostrum, contains vitamins, enzymes and antibodies.
Experts say that lactation itself does not affect the shape of the breast in any way. If a woman is healthy, takes proper care of her breasts, then the shape will remain the same.
The change in weight during pregnancy mainly affects the beauty of the breast. The natural elasticity of the skin is quite enough for it to “withstand” the increase in the mammary glands during the feeding period. However, if a woman gains excess weight during and after pregnancy, the breast skin experiences even greater stretching. As a result, the skin cannot cope with such loads, and stretch marks appear. And when a woman loses weight again, the stretched skin and ligaments of the breast may no longer take their former shape, and the breast will “sag”, the stretch marks will remain. In women with a small size of the mammary glands at the end breastfeeding it may seem that the breast has become smaller - the reason for this is also a change in the shape of the mammary gland. So the only way to save beautiful breasts- carefully monitor your diet and try to keep your body weight normal.
Breast care while breastfeeding
The restructuring and preparation of the mammary glands for lactation begins from the first days of pregnancy as a result of a complex interaction of hormones of the ovaries, placenta, pituitary gland, thyroid gland, and adrenal glands. Contrary to popular belief, the breast does not need any special preparation for the feeding process. Neither wearing a bra, nor pouring and hardening the breast, nor rubbing the nipples during pregnancy affect the success and effectiveness of breastfeeding. On the contrary, such procedures can cause additional trouble for the expectant mother.
For example, wearing a bra is not always justified if a woman has small breasts or very sensitive skin. The bra solves cosmetic and aesthetic problems, does not allow the breast to sag, supports it, protects large breasts from stretch marks, but does not affect the formation of milk in any way. Therefore, special attention must be paid to the breast during lactation.
After childbirth, the amount of milk produced is determined by the concentration of the hormone prolactin, the secretion of which increases under the influence of the sucking movements of the child. The level of lactation depends on the frequency of attachment of the baby to the breast, on the needs of the baby.
In the process of milk secretion, two phases are distinguished. In the first, associated with irritation of the receptors of the mammary gland, the sphincters of the nipple-ariolar apparatus (circular muscles that "lock" the excretory ducts) are relaxed and the milk ducts are activated. So-called "early milk" of low fat content comes out. In the second phase, the hormone oxytocin is released from the pituitary gland (an endocrine gland located in the brain), which causes the glands to contract, which ensures the removal of more fatty “late milk” from the mammary gland. It is important to completely empty one gland in one feeding and only after that the baby can be applied to the other breast .
If you take a shower every day, then you should not wash your nipples before and after feeding. Soaps and disinfectants can dry them out, predisposing them to cracking. You also do not need to lubricate the nipples with a solution of brilliant green ("brilliant green").
The structure of the mammary gland
The mammary gland is formed from 15-25 lobes separated by connective septa and adipose tissue. Each lobule has ducts and terminal vesicles that produce milk. The hormone progesterone stimulates the development of the glandular elements of the breast tissue from the very first days of pregnancy: under its influence, the terminal vesicles increase in volume and become larger. At this time, the woman feels engorgement and slight soreness of the chest. 2-3 days after birth, the pituitary hormone prolactin, which is responsible for milk production, comes into play.
To avoid problems...
In the first days after childbirth (until milk has come), the mother should not drink a lot of fluids. You need to limit yourself to 600-800 ml (including soups, milk drinks, etc.), otherwise formation may occur. a large number milk, and this, in turn, will lead to lactostasis - stagnation of milk.
Many women who have given birth, unfortunately, are familiar with the condition when the breasts swell and become painful, and seals appear in the mammary glands. It may even rise in temperature. This is lactostasis. As already mentioned, the mammary glands resemble orange slices, connected by narrow ducts through which milk enters the nipple. If milk is produced too intensively or the ducts do not pass it well, the milk, as it were, “overflows” the lobules and stagnates in them.
By itself, lactostasis is not a disease. But stagnant milk is a beneficial environment for the development of microbes, therefore, if an infection gets into the crowded lobules, inflammation may begin - mastitis. And this is a dangerous disease that requires urgent medical intervention. To avoid it, make sure that there are no stagnations anywhere. If you notice a painful engorgement in some part of the breast that does not disappear after feeding, you need to massage the breast in a circular motion from the periphery to the center, express the remaining milk until a feeling of comfort appears.
Another very common complication that occurs in young mothers is cracked nipples. It is through them that the infection that causes mastitis most often enters the body. If cracks have already appeared, it is necessary to treat them regularly (after each feeding) with special preparations (they are sold in pharmacies - PURELAN, BEPANTEN) and change linen more often.
The reason for the appearance of nipple cracks is, first of all, the incorrect attachment of the child to the breast, when the baby captures only the nipple, but not the peripapillary pigmentation. In addition, the formation of cracks is promoted by frequent washing of the breast, as well as the use of alcohol-containing solutions for the treatment of the nipple and areola, since such procedures lead to the "drying" of the areola and nipple. Improper breastfeeding by the baby causes unpleasant and sometimes painful sensations in the mother, therefore, even slight discomfort during feeding requires very active attention, being evidence of the inadequacy of the chosen method and feeding technique. If this signal of trouble is neglected, then soon reddening of the skin may appear on the nipple at the site of soreness, and then a crack. Therefore, it is important not to miss the time when there is still an opportunity to prevent its occurrence by changing the technique of feeding the child, once again checking the correctness of the baby's capture of the breast. Already at this time, you need to use the above drugs.
Another common cause of nipple injury is improper weaning of the baby at the end of a feed. It is unacceptable to remove the nipple in the presence of a squeezing force or sucking of the child, as this may injure the skin of the nipple. It is necessary that the child himself release the nipple by opening his mouth. For proper weaning, you need to insert your finger into the corner of the baby's mouth, between the two gums, unclenching them so that the nipple comes out of his mouth.
After feeding the baby, to prevent the formation of cracks, squeeze a little milk out of the nipple, grease it evenly on the nipple and areola and let it dry for 3 to 5 minutes. Milk contains enough active substances that can promote the healing of cracks. Additionally, for prevention, you can regularly use creams consisting of 100% lanolin, which does not require rinsing before feeding. Avoid creams and ointments that need to be washed off. Antiseptics, aloe juice, beeswax oil that were previously widely used to lubricate the skin are not recommended, as the baby may not like their smell.
If the fissure does not heal within 2-7 days, then it is necessary to stop applying the child to the sore breast for at least 1-3 days. At the same time, the child can be full, receiving only one breast, and in some cases he will need to be fed from a spoon with milk expressed from a diseased gland (the baby is recommended to be fed from a spoon, and not from a bottle, because after the pacifier the baby may refuse to breast). After a few days, you can return to the application, but at first - using the diseased breast as an addition to feeding from a healthy one. If cracks appear on both mammary glands, depending on the severity of the cracks, you can either continue feeding, or put the baby to the breast for a short time, and then feed with expressed milk from a spoon, or feed only expressed milk. If there are cracks, silicone breast pads can be used to reduce soreness, but it will be more difficult for the baby to suckle. Do not use overlays all the time. Also, if you are producing a lot of milk and leaking from your breasts between feedings, it is better to use porous reusable pads or special ventilated milk pans (reservoirs that fit in a bra), they will collect excess milk and allow the nipple to dry out. If the nipple remains constantly wet, the risk of irritation, infection and cracking increases.
So, the health and beauty of the breast is in your hands. You can save the shape of the bust after lactation! Proper breast care during pregnancy and lactation, gradual (rather than abrupt) cessation of feeding, proper diet and moderate exercise will all help keep breasts healthy and attractive. Statistics collected by scientists suggest that women who breastfeed their children are much less likely to experience mammological problems than those who do not breastfeed. A woman who breastfeeds is at a lower risk of anemia (anemia), ovarian (adnexal) and breast cancer, and other diseases. This is due to the natural restoration of hormonal levels after childbirth and a number of other factors.
Is topless tanning harmful?
Doctors generally do not advise sunbathing with an open chest - strong sunlight is harmful to the delicate skin of the chest. During pregnancy and lactation, you should be especially careful with the sun: firstly, it is not very useful, and secondly, sunburn can provoke the appearance of age spots.
“I’m afraid that my breasts will sag after giving birth,” such fears can often be heard from expectant mothers. What changes occur to the mammary glands during pregnancy and after childbirth? How to properly care for and care for the breasts of a nursing mother - says mammologist, doctor of the highest category Natalya Leonova.
Pregnancy is a wonderful time in a woman's life. But the expectant mother is worried about what will happen to her breasts after childbirth and feeding.
Few people manage to keep their breasts beautiful after childbirth without making any effort. A good breast shape is genetically determined, and, unfortunately, not every woman can boast of such heredity. Pregnancy is hard work for the whole body. After the end of the period of gestation and feeding, a woman often expects sagging breasts and stretch marks on the skin, which can usually be eliminated only with the help of surgery. So what to do? Deprive yourself of the most important stage in life? In no case! You just need to start taking care of the beauty and health of your breasts from the very first days of pregnancy.
beauty takes time
The breast of a woman begins to prepare for a meeting with the baby at the very beginning of pregnancy. The process of breast enlargement proceeds unevenly.
- In the first ten weeks, the breast increases quite quickly, then the process stops for two to four weeks, and then the development of the mammary glands resumes, gradually increasing.
- By the end of pregnancy, the volume of each breast increases by about 200 ml.
- Simultaneously with the increase in the mammary glands, changes in the nipples and areolas are observed: the diameter of the areolas increases on average from 35 to 51 mm, and the nipple itself - from 10 to 12 mm. The nipple becomes more elastic and mobile.
As the mammary gland grows, the load on the skin also increases. The higher the skin tone, the more it has the opportunity to return to its original state. The more elastic the skin, the less likely it is to develop stretch marks. You can maintain skin tone with the help of special creams that contain vitamins A and E.
- The elasticity of the skin also depends on the nutrition of the woman. And we are talking not only about the composition of the menu, which must necessarily include foods rich in vitamins A, E and C (fruits and vegetables of orange and green), but also about the diet in general. After all, if a woman gains excess weight during pregnancy, the breast skin experiences a double load. Not only does the volume of the glandular tissue of the mammary gland increase, but the fat volume also increases. As a result, the skin cannot cope with such loads, and striae (stretch marks) appear. And when a woman loses weight again, the stretched skin and ligaments of the breast may no longer return to their previous state - the breast will “sag”, but the striae will remain. In addition, adhering to the principle “I eat everything I want for two”, we enter in advance a considerable list of chronic diseases in the anamnesis of the unborn child.
- Another thing you need to keep your breasts in shape is a good bra with wide straps, made from natural material. It supports the chest and protects the skin from possible stretching. Incorrectly fitting underwear can harm the mammary gland. Traumatization of the chest by bones cutting into the body can cause the development of oncological diseases. Underwear should support, but in no case tighten the chest, interfering with the full blood supply. Poor nutrition of the vascular tissue can lead to various kinds diseases. As the mammary glands increase, it is necessary to change bras to other, larger sizes.
Do pregnant women need to wear a bra all the time - the opinions of doctors here sometimes do not coincide. Some advise wearing it without taking it off. Others spend enough time (mostly at home) in a "free state": the chest also needs rest.
With active walking, running, and other physical activities, it is very important to use a comfortable bra to protect the chest from concussions, which increase the risk of stretch marks and sagging. And, finally, a beautiful breast shape depends not only on the readiness for skin loads, but also on the state of the largest pectoral muscle and the ligamentous (breast-supporting) apparatus. During pregnancy, it is not recommended to engage in strength exercises, but a moderate sports load for the expectant mother will be very useful. If the pregnancy is proceeding normally and the doctor does not mind, you can sign up for a pool or special gymnastics for pregnant women, yoga.
Preparation and medical supervision
If advance care of the skin, muscles and ligaments will help maintain the shape of the breast later, then taking care of the nipples during pregnancy is a guaranteed protection against possible mastitis (an inflammatory process in the mammary gland that begins due to the appearance of cracks in the nipple).
From the first days of pregnancy, you need to start gently massaging the nipples, slightly pulling them out with two fingers. This will prepare the nipple to perform its functions, make the skin around it hardy, and the shape of the nipple more comfortable for the baby. The baby will naturally accept the "prepared" breast, and it will not be injured.
The nipples will also be hardened by regular washing with room temperature water.
You can gently massage your breasts with a terry towel.
And, of course, during all nine months it is necessary to be observed by a mammologist, especially if any abnormalities or diseases of the mammary gland were found in a woman before pregnancy (or in her maternal relatives).
There is an opinion that some mammological diseases are “cured” by pregnancy. This is wrong. But most benign neoplasms are not a contraindication for pregnancy and lactation (the vast majority of women suffer, for example, from fibrocystic mastopathy). The doctor will simply observe the woman during pregnancy with the help of ultrasound. If a woman has cysts, it is very important not to expose yourself to drafts and hypothermia, so as not to cause an inflammatory process in the mammary gland.
The only disease that requires medical monitoring during the entire pregnancy is fibroadenoma,
benign hormone-dependent breast tumor.
In this matter, doctors are categorical: fibroadenoma not only does not “resolve” during pregnancy - unfortunately, under the influence of hormones during this period, it can become more active in growth and even develop into a malignant one. A woman suffering from fibroadenoma, when planning a pregnancy, must definitely consult a doctor (mammologist, oncologist, gynecologist-endocrinologist). Most likely, the doctor will offer her to remove the tumor on the eve of pregnancy, and in the case of multiple fibroadenomas, he will also prescribe treatment from a gynecologist-endocrinologist (since it will first be necessary to normalize the level of hormones so that new fibroadenomas do not occur).
If pregnancy caught a woman with this disease by surprise, she now simply needs constant medical supervision. Except in the case of fibroadenoma, doctors categorically do not recommend giving birth with breast cancer.
But women who have undergone a mastectomy (an operation to remove the mammary gland) have every chance of becoming a mother (even a nursing one). But of course, these cases are purely individual and require constant medical monitoring.
During pregnancy, you need to think not only about childbirth, which passes very quickly, but also about the upcoming breastfeeding, because it is this that determines whether your postpartum milk period will be favorable or unfavorable.
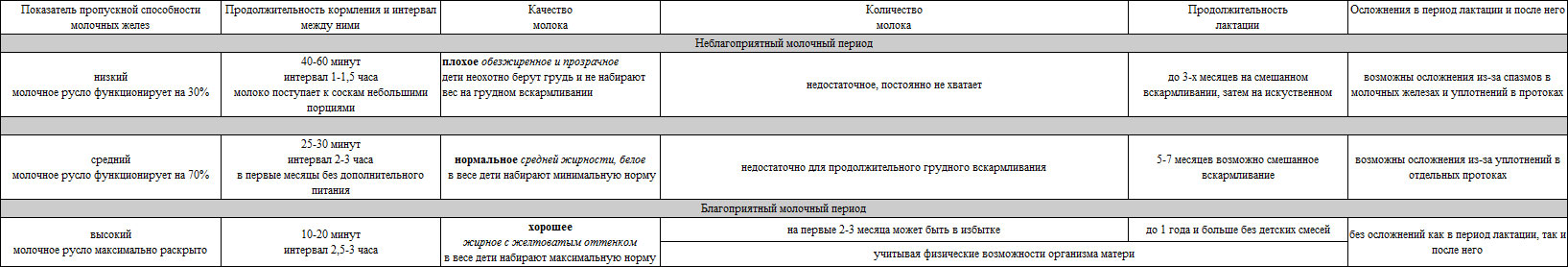
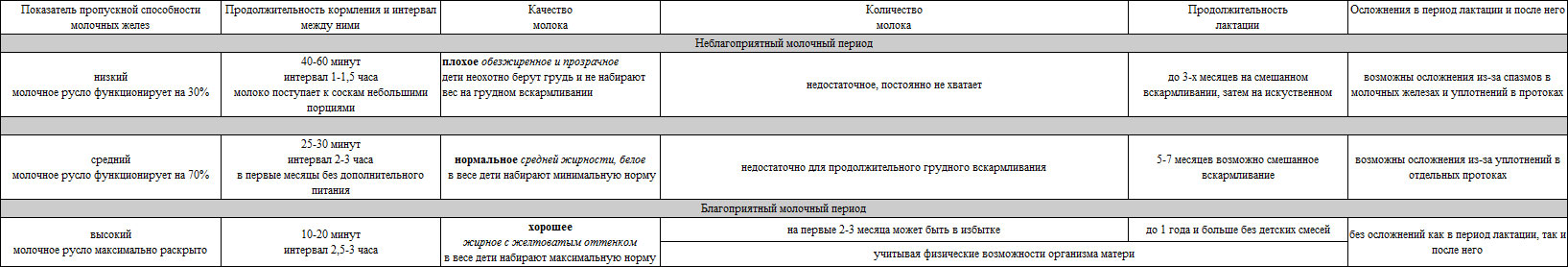
The table below shows what the milk period is like in the life of a mother and her child.
The maximum disclosure of the entire milk channel in the postpartum period (i.e. its recovery) allows you to maintain a favorable milk period for a long time. This is a reliable prevention of all postpartum complications in the mammary glands.
As practice shows, milk production, its quality, quantity and duration of lactation mainly depend on the throughput of the mammary glands. And therefore, if the entire milk channel is maximally opened during lactation, then 8 out of 10 nursing mothers can breastfeed for up to a year or more.
The table below shows what the milk period is like in the life of a mother and her child.
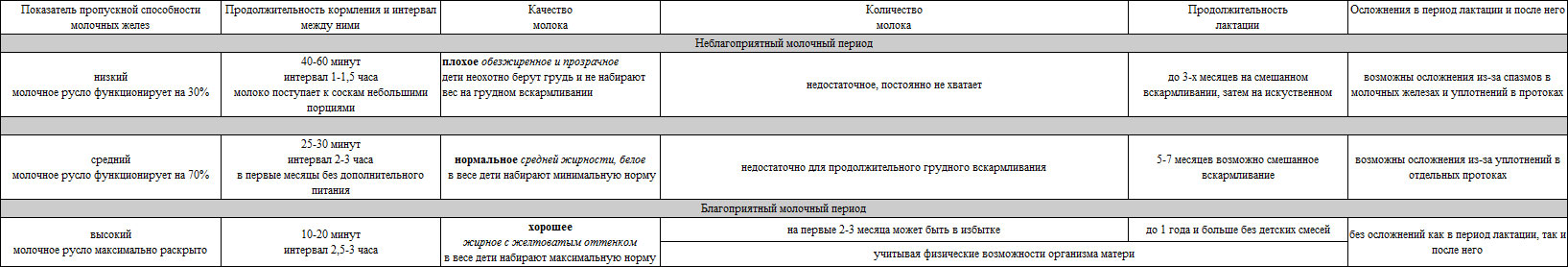
After reading the table, the question may arise: why is there such a different throughput of the mammary glands? Initially, much depends on the state in which they were before and during pregnancy. Starting from the second half of pregnancy, the mammary glands change their shape, filling with colostrum, increase in size, thicken, thus experiencing additional physical activity. This discomfort of the mammary glands is always accompanied by initial hypoxia (oxygen starvation) due to a slight violation of blood circulation. Such a state of theirs can be aggravated when such spasms turn into densities. On palpation in such mammary glands, painful areas are determined. In order to avoid excessive overloads in them, it is necessary during pregnancy to prevent hypothermia of the body, especially to avoid drafts that adversely affect the mammary glands.
A very big obstacle to the upcoming lactation are various seals, mastopathy, etc., which can appear even before pregnancy. Such compacted areas constantly experience hypoxia and in some of them the milk ducts may already be closed. Contributing factors for such seals are: abortion, hormonal disorders, chronic gynecological diseases, as well as an unfavorable previous milk period with short lactation and seals on closed milk ducts.
In the postpartum period, approximately on the third day after a strong influx of colostrum, the mammary glands experience the greatest physical load. In order for lactation to take place, they need to withstand this load, then skip the colostrum to the nipples in a timely manner and as close as possible. But through various kinds of elasticity before pregnancy, as well as their spasms and seals during pregnancy in the postpartum period, after the influx of colostrum, excessive tension and painful seals of the mammary glands occur, which in turn leads to a decrease in the throughput of the milk ducts. This becomes noticeable immediately at the beginning of lactation, when the colostrum enters the nipples is no longer transparent, but orange, but in a small amount, the child constantly lacks it. In the future, due to the low throughput of the milk ducts, the entire milk channel cannot open to the maximum, which negatively affects the further production of milk. From here, an unfavorable milk period begins, most women in labor fall into a similar situation.
During lactation, the nipples are a mirror of the mammary glands. The main sign of insufficient functioning of the mammary glands is the overload of the nipples from the first postpartum days. The closed ducts in the hard mammary glands prevent the nipples from moving during feeding, so the nipples are easily chewed and swollen. As a result, the child is not able to properly (i.e. completely) capture such a sedentary nipple, poor feeding always takes a very long time: the nipples, unable to withstand excessive stress, begin to become inflamed, after a while cracks appear on them. And no prenatal recommendations for nipple hardening will help here.
Through inflammation of the nipples, spasms in the mammary glands and seals in the ducts, the child constantly lacks quality milk, and over time, accordingly, its quantity is lost; milk comes to the nipples slowly, in small, fat-free portions. Babies suckle actively for only 5-7 minutes, while milk comes to the nipples, then there is “empty sucking” (there is no milk flow, and the children actively chew on empty nipples). Due to inflammation of the nipples, the milk channels in them narrow, which further complicates the outflow of milk and leads to a gradual accumulation of fats in the milk ducts. After some time, the channels may completely lose their capacity. Milk, which used to flow more freely from the alveolar milk bed through the ducts to the nipples, now begins to stagnate, and the mammary glands painfully thicken. At the same time, the bloodstream always suffers (it stagnates at the capillary level). In this condition of the mammary glands, inflammation of the ducts may increase, and painful seals, increasing gradually, will turn into a general tight spasm (lactostasis). If help is not provided in time, milk fever may be connected to lactostasis, followed by mastitis. Of the mammary glands poorly prepared for lactation, children eat for a long time (40-60 minutes), do not eat up and fall asleep half-starved, tired. With prolonged feeding, the interval between feedings is always reduced (up to 1-1.5 hours) due to the insufficient amount of milk consumed. Children with such feeding practically do not gain weight.
With any of the lactostasis, a rapid increase in hypoxia occurs. And if this is a primary stagnation in colostrum (which appears even in the maternity hospital), then at least there will be painful seals in the mammary glands. This condition of theirs cannot last long, it is urgent to provide assistance. But it is not easy to cope with such lactostasis, because stagnation in colostrum is always stronger than in milk. In order to avoid major complications, women in labor in maternity hospitals are advised to limit fluid intake, which to some extent reduces the flow of colostrum, but this is not always useful. If the milk channel at least a little passes colostrum to the nipples, then the more the child eats it, the better it will be both for him and for further lactation. Therefore, if it is sometimes necessary to limit the fluid consumed, then it is purely individual. With severe lactostasis in the maternity hospital, they can always provide assistance that will stop inflammation, and swelling and cracks in the nipples will decrease after the use of antiseptic ointments. A gradual decrease in lactation will reduce the threat of further inflammation, so it is rare for anyone who has given birth in the postpartum period to have purulent mastitis or milk fever.
Due to primary lactostasis, children do not receive the required amount of colostrum, so in maternity hospitals they are forced to supplement with mixtures. In the future, if you do not improve the mammary glands, they will not be able to function normally. The production of prolactin, which is directly involved in lactation, will gradually decrease.
An insufficient amount of milk produced disrupts the normal feeding regime, so many children in the first month of life have dyspepsia (an upset of the gastrointestinal tract) and lag behind in weight. All this appears for a simple reason: if the child does not eat up in 30 minutes from two mammary glands, then he does not have enough milk (this is the main reason for the child to lag behind in weight). Holding the child near the breast for up to 1 hour leads to dyspepsia, because after half an hour the milk that entered the stomach, turning into cottage cheese, continues to flow into the intestines. If you feed your baby for more than 30 minutes, then even a small portion of fresh milk, mixed with cottage cheese, then leads to bloating and colic. This reduces the child's appetite, causes sleep disturbance, such children are restless and capricious. Due to inexperience, parents, not seeing a way out, begin to feed their children every 1-1.5 hours, not knowing that frequent feeding puts a strain on the intestines and can increase intestinal colic.
Of course, you need to feed the baby on demand, but on the condition that your baby is full of breast milk for a maximum of 20-30 minutes. and maintains an interval of 2.5-3 hours. It will be on-demand feeding as it should normally be. With such feeding, the child may not even be weighed, he will definitely gain monthly normal weight. But if your child does not eat at the right time, you need, first of all, to adjust the feeding (to decide whether to continue feeding with mixtures or to establish breastfeeding). In order to quickly and maximize the possible production of milk, my advice to you is to look for a competent lactation specialist, because until the milk channel opens up to the maximum, no means of increasing lactation will help you, and milk will not be added.
Let me give you a simple example: if your child is 2 weeks old, and you keep him near your chest for up to an hour, while not feeding anything, this means that the child may already have dyspepsia and weight loss. He urgently needs supplementation. Having eaten up, such a child can wake up for the first week and require supplementary feeding after 2 hours, until he catches up with the lost weight. Gradually, the interval between feedings normalizes to 2.5-3 hours. If the child still has dyspepsia, he can wake up 1-1.5 hours after feeding. In this case, the child should be regularly given unsweetened baby tea or dill water between feedings. If the child continues to act up, it means that his stomach is still swollen. A good and easiest way to get rid of intestinal colic is to use a baby pear with a pre-cut bottom (1 cm in diameter), the tip of the pear should be rubber. Such a pear will serve as a good gas outlet, the advantage of which is that it can be used several times within 1-2 minutes, after washing it under running water and lubricating the tip with boiled vegetable oil before each use.
First of all, I want to draw your attention to the fact that in a favorable milk period with the maximum open milk channel (taking into account the physical capabilities of the mother's body to produce high-quality milk), the above definitions lose their meaning. And now about all this in order.
Through dense milk ducts and inflamed nipples, skimmed milk, which is also called immature or fore milk, passes. It comes to the nipples in small portions. And in order to somehow feed the child, the mother holds him near her chest for about an hour (you already know what follows from this). Due to inexperience, such protracted feedings can last a maximum of a month, but not more, because exactly after 1 month you will go to the pediatrician's clinic for examination and weighing of the child, and there you will learn about your first milk crisis, because. due to insufficient milk, your baby will not gain normal weight and you will definitely be offered to supplement the baby with mixtures. In the second month of mixed feeding, 2 undesirable factors will appear: artificial supplementary feeding, and the second - a psychological factor. A child, having tried a bottle from which it is easy for him to suck, may at first be reluctant to take a breast from which it is more difficult to suck. Lactation will always decrease if the child no longer has the need and desire to suck milk to the end. Thus, if urgent measures are not taken, breast rejection may gradually occur, and every day you will lose hope of breastfeeding more and more, classifying yourself as a “non-dairy mother”. In order not to completely lose milk, you need to compete for lactation, otherwise by 3 months it may completely end. This will be the second milk crisis, irreversible for many. Children with such low lactation are often unreasonably called lazy suckers.
Some authors claim that problems with the mammary glands appear due to the large amount of milk in them. This is quite possible, provided that such an amount of milk constantly stagnates in the mammary glands due to the reduced throughput of the ducts. But if there is a lot of milk and it moves freely to the nipples during feeding, then good milk pressure in the glands will help the child to eat up in 10-15 minutes from one mammary gland. This is a very good indicator of lactation, which can last more than a year. With good and prolonged functioning of the mammary glands, even prenatal mastopathy can resolve in them (if the milk channel is maximally opened in such a compacted area). There is such a pattern: in women who have given birth, the milk ducts should normally always be softer than in those who have not given birth. In a favorable milk period, with good lactation (on an open milk channel), the milk ducts acquire their natural physiological relaxation in 1.5-2 months, become more mobile and elastic. This gives them the opportunity to always be in good condition, both during lactation and after it. But if during lactation the milk ducts did not function well, then instead of relaxing, they will thicken and become denser than their prenatal state until the end of lactation. Such excessively compacted areas constantly experience hypoxia, which is very undesirable for them in the future.
In the postpartum period, all problems with the mammary glands begin after suffering primary lactostasis. First, lactation decreases, this leads to weight loss in the child. In the future, an insufficient amount of milk produced makes it necessary to supplement with mixtures, which in turn creates an additional burden on the child's gastrointestinal tract. Mammary glands unprepared for lactation can be subject to various complications. There is only one way out of this situation - to feed the child from the first days of his life only with colostrum, and then only with milk. For most women in labor, this is quite possible, provided that they do not have any postpartum problems with the mammary glands. The most effective way to deal with all postpartum complications in the mammary glands will be the timely prevention of such complications.
The preventive comprehensive preparation of the mammary glands for lactation, which I developed, starting with a one-time prenatal session with individual recommendations, will enable each woman in labor to prepare the mammary glands for colostrum immediately after childbirth, with further proper care for them. The mammary glands prepared for colostrum will painlessly go from non-working to working state (avoiding primary lactostasis, inflammation and cracks in the nipples). Your child from the first days of life will take the breast, and will be able to eat only colostrum, which is very important for him; at the same time, the throughput of the mammary glands can already be more than half. From here, a favorable milk period originates, which must be fixed while already at home, having timely prepared the mammary glands for further good lactation (opening the entire milk channel in them as much as possible). This will give you full control over the process. breastfeeding and will in no way allow the child to lag behind in weight.
Timely prepared for lactation, the mammary glands are able to maintain lactation at a good level for a long time. Normally, the mammary glands should be firm before feeding and relatively soft and painless after feeding. In a favorable milk period, there are no milk crises, sometimes there can only be a short-term decrease in lactation for some reasons:
In this period, with good lactation, colostrum first appears in the form of transparent drops, the child only needs to lick it regularly. On the second day, there will already be more colostrum, and the child’s gastrointestinal tract will prepare for normal functioning during this time. By feeding colostrum from the first days, you strengthen the child's immunity and protect him from intestinal disorders (including dysbacteriosis). A sufficient amount of colostrum indicates a good initial functioning of the mammary glands. This helps to improve uterine contraction in the postpartum period, which in turn enhances the flow of milk (prolactin is more actively produced, which is necessary for the normal functioning of the mammary glands). After colostrum, after a few days, transitional milk will appear, no longer as orange as colostrum, but with a yellowish tint; it will be more than colostrum. And after 3-4 days, milk will arrive without delay. Of the mammary glands well prepared for lactation with active sucking (if the child is not disturbed by the intestines, and he breathes well through the nose), babies eat up in 10-20 minutes from one mammary gland and maintain an interval between feedings of 2.5-3 hours. This is normal lactation children will gain weight well. With such lactation, there will no longer be the need to feed the baby at night. The interval between feedings from 24-00 to 5-00 will benefit both the mother and the child. For a baby this is an unloading of the intestines, and for a nursing mother a good rest is an increase in milk production.
The mammary glands, in which the entire milk channel is maximally open, can not only maintain existing lactation, but also significantly increase its level. At the same time, children receive high-quality and affordable milk, and the mammary glands receive oxygen and nutrients in a timely manner and in sufficient quantities. Such functioning will reliably protect the mammary glands from possible congestion, inflammation and further complications.
Care for breasts prepared for lactation takes very little time 0.5 minutes before feeding and 3-5 minutes after.
Remember! Only with the maximum opening of the entire milk channel is a good and long lactation possible. This is necessary not only for the health of the child, but also for the health of the mother both during lactation and after it.
1. Protect nipples from overload (inflamed nipples make it difficult for milk to flow out).
While in the hospital, feed the baby for no longer than 10 minutes from one breast and a maximum of 30 minutes from both;
When already at home, do not apply the child unnecessarily to the nipples (when he is worried about the intestines), it is better to give him baby tea.
2. In the first postpartum days (3-5 days), drink liquids no more than 1.5 liters per day, in the future, to maintain good lactation, as needed.
3. Make sure that the baby breathes well through the nose during feeding, this increases the activity of sucking and reduces the swallowing of air.
4. In any situation (reddening of the mammary glands, fever up to 380C), you can apply a cooling compress to the chest while taking antipyretics.
5. In the case when you need to stop lactation, do not tighten the glands this can cause a number of complications. It would be correct to reduce lactation gradually, using special means, simultaneously applying a compress with camphor oil for a certain time (taking into account the residual amount of milk in the mammary glands and the condition of the milk ducts).
A common situation is the allocation delay process breast milk after childbirth. Especially this issue concerns primiparous women who do not have the skills of breastfeeding and its organization. This problem is not a serious pathology, since it is based on only a slight slowdown in the physiological process, which can be corrected through some recommendations.
The formation of congestion in the mammary glands not only creates an obstacle to breastfeeding, but also gives a woman a lot of discomfort and even pain. The main manifestations of breast milk stagnation are hardening of the mammary glands, the appearance of soreness and a feeling of fullness. When pressing on such a breast, a drip of small portions of breast milk may be observed.
The main reasons for the formation of congestion in the mammary glands are:
As another, no less likely cause of lactostasis, one can single out excessive production of breast milk in the first few days after childbirth.

The primary task is to choose the correct position of the body of the mother and child during breastfeeding. Attachment to the breast is recommended to be carried out in such a way that the child's chin is in contact with the area of \u200b\u200bthe mammary gland in which the woman feels maximum discomfort and pain. If there are stagnation in the lower part of the gland, then the position of the child during feeding should be sitting on the mother's lap.
With median stagnation of breast milk, the position of the mother during feeding should be on her side, applying the baby to the breast that is on top.
In order to develop breasts after childbirth in the shortest possible time and painlessly, it is necessary to put the baby to the breast as often as possible, and feed in small portions.
If the breastfeeding procedure does not contribute to the normal outflow of milk, a woman needs to carry out manual pumping.
Important! With an increase in body temperature and the appearance of a sharp soreness in the area of \u200b\u200bthe mammary glands, it is strictly forbidden to use manual pumping methods. A woman should immediately contact a medical specialist.
The development of the mammary glands in the postpartum period is carried out according to the following scheme:
If the body temperature is within the normal range, and there is no sharp pain, then in no case should you stop breastfeeding.
The negative pressure that occurs between the baby's mouth and the mother's nipple promotes accelerated drainage of the mammary glands. The pressure of the baby's chin on the mother's breast is an effective massage that stimulates the expansion of the ducts and the release of milk.

To quickly and effectively develop breasts after childbirth, you can use the technique of a special massage. If the woman's nipple is not prominent enough, then the primary task of the massage is to eliminate this problem. To do this, you need to slightly pull each nipple with two fingers and gently massage. A similar massage is performed daily in several approaches.
To simulate the discharge of breast milk, it is necessary to perform the following massage techniques:
Proper care of the mammary glands helps to normalize the outflow of milk after childbirth. It is recommended to wash the chest with warm water before and after feeding, wiping dry. If small cracks appear on the nipples, it is recommended to lubricate them with baby cream after feeding and taking a shower.
In the absence of positive results, it is necessary to contact a medical specialist who will identify the causes of such stagnation and prescribe treatment. Self-medication can cause a number of side effects.